Pain Profile: Gluteal Tendinopathy
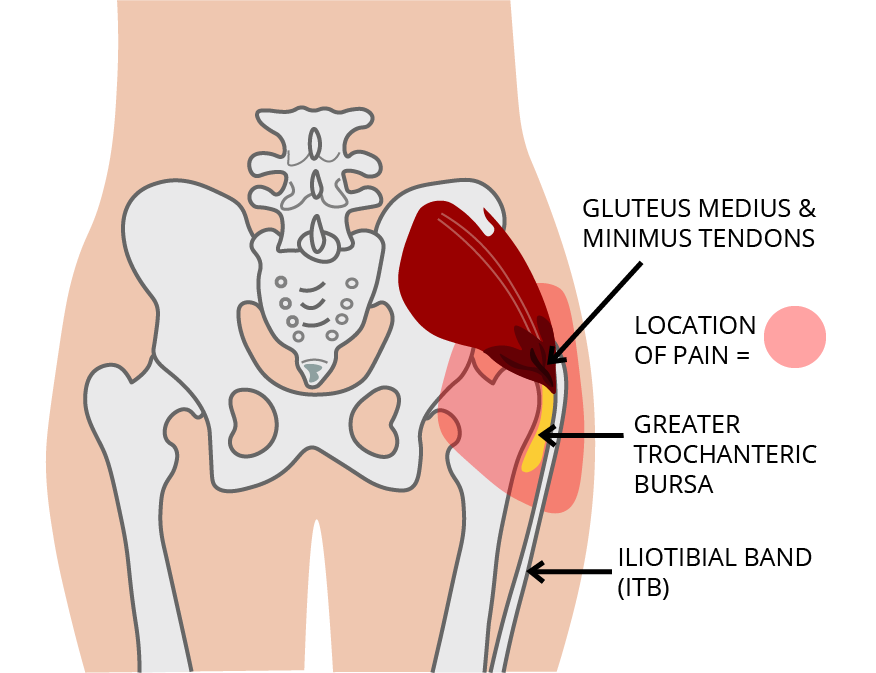
Lateral hip pain can have many causes, but one of the most common sources comes from a tendinopathy of the gluteus medius and gluteus minimus muscles. Traditionally this pain presentation was often diagnosed as Greater Trochanteric bursitis, but research has found that any pain associated with the bursa is normally secondary to a tendinopathy. This grouping of conditions is sometimes referred to as Greater Trochanteric Pain Syndrome (GTPS). Similar to the Plantar Fasciopathy, this condition is considered to be degenerative as opposed to inflammatory.
Mechanism of injury
Mechanical loading within the tendons of the gluteus medius and minimus muscles appears to be one of the key components in the development of Gluteal Tendinopathy. Under constant load, these tendons will undergo changes as a cellular level which can impact on their ability to load-bear. Tendon loads are at their highest when the muscle is active and being lengthened at the same time. With gradual increases in load combined with sufficient periods of rest, these tendons will actually have increases in their load-bearing capacity. A rapid increase in intensity and/or frequency of load on the tendons is what leads to gluteal tendinopathy developing. Decreased loading of the muscle tendon combined with compression can also lead to symptoms developing. The compression combined with the decreased stress on the muscle actually leads to certain collagen fibres breaking down and predisposing the muscles the injury under lower levels of load.
Hip Pain: Gluteal Tendinopathy as Greater Trochanteric Pain Syndrome (GTPS)
Signs and Symptoms of Gluteal Tendinopathy
Pain and tenderness around the lateral hip, particularly over the greater trochanter
Moderate to severe pain
Pain can refer into the buttock, groin or down the outside of the leg just below the knee
Pain is worse at night while trying to sleep, particularly for those that sleep on their sides
Getting up from sitting down for a long period of rest can also bring on lateral hip pain
General weight-bearing activities such as walking and standing can also cause pain depending on the severity of the condition
Other activities that can aggravate pain include walking up hills/stairs or standing on one leg while getting dressed
Predisposing Risk Factors
Age & Gender - Gluteal tendinopathy is more common in females than males (3-4:1) with likelihood increases beyond the age of 40. Changes in oestrogen levels is related to the health of collagen fibres, especially pre-post menopausal.
Conditioning - Introduction of new physical activities with increased load around hip musculature after sedentary periods.
Terrain - Young athletes involved in activities like hill running or repetitive high stepping. Running the same direction around a track, up hills or on uneven surfaces.
Posture - Habitual postures involving increased hip abduction (saddle chairs) leading to tightness around lateral hip.
Poor postural and movement habits
Standing, hanging on one hip - increased hip adduction and using the iliotibial band (ITB) to support weight through hips.
Not using gluteal muscles to stabilise hips which lead to biasing of the superficial muscles (tensor fascia latae and upper gluteus maximus) which further increases compression.
Sitting with legs crossed or with knee together and feet spread.
Post accident - After a slip or fall leading to a strong contraction of the hip abductor musculature.
Leg length difference – increasing hip adduction on long leg side.
Femoral neck angle – increased angle of the neck of the femur means increased compression of ITB over greater trochanter.
Scoliosis affecting hips - changing of hip heights similar to leg length difference.
Gait/Biomechanics - Running with your feet tracking towards or past the midline of your body.
Abdominal fat – increased likelihood of tendinopathy.
Over-stretching of the lateral hip - increases compression on the area.
Differential Diagnosis
What else could it be?
Lumbar pain - the L4 nerve root pain refers to the lateral hip. A thorough history and assessment of the lumbar spine will help rule differentiate between the two.
Hip osteoarthritis - degeneration of the hip joint cartilage and tissues. Some suffering with hip OA will generally have difficulty putting on shoes and socks while someone with Gluteal Tendinopathy will not.
Labral tear - the hip labrum is a ring of cartilage that goes around the socket of the hip providing cushioning for the joint while sealing the head of femur into place. Clicking in the joint is common with labral tears.
Treatment and Rehabilitation
The first step in treating Gluteal Tendinopathy is education around the condition and why it is presenting, specific to the patient. Acknowledging the predisposing and aggravating factors can allow the patient to better control their symptoms and reduce aggravation of pain right through their rehabilitation. Better understanding of the mechanisms of the condition can allow the patient to avoid tendon compression and continue with their exercise program.
If muscle tension is present, avoid trying to stretch the area. This only leads to more compressive load on the tendons. Massage and trigger point release can be beneficial for symptomatic pain relief and reduction is resting muscle tone. At home, using a spiky ball on the lateral hip muscles can provide some relief while heat is also an option. One of our therapists will show you how to do this effectively.
Altering your sleeping postures to decrease load on the lateral hip can also help to improve night pain and improve sleep quality. Laying on your back with a pillow under your knees is one option. If you can only sleep on your side; sleeping on the affected side, try using an eggshell mattress topper and for sleeping on the unaffected side, propping your top leg up with a pillow so that the knees and hips are closer to horizontal (see picture).
Positions and activities to avoid include:
Standing hanging on one hip in adduction.
Sitting with legs crossed.
Sitting with the feet wide and knees together.
Sitting with hips in more than 90-degree flexion, hips lower than knees (low lounge, car seats)
Stretching will aggravate the pain around the hip and should be avoided
Corticosteroid (Cortisone) injections* have been found to have good short term effects on Gluteal Tendinopathy pain but will start to wear off after around 3-4 months with long term effects deemed to be poor. (*Not administered at Upside Health & Movement)
Recovery time for this condition ranges from patient to patient depending on the individual's presenting history, severity of symptoms and their compliance to rehabilitation.
If you are suffering from lateral hip pain and think it might be caused be a Gluteal Tendinopathy, book in a session with us at Upside Health & Movement and we will get those hips back on the right track.
References:
Grimaldi & Fearon (2015). Journal of Orthopaedic & Sports Physical Therapy, Volume 45, Issue 11, pp 910-922.